ARKANSAS HEART HOSPITALA Bastion of Scientific Rigor in Indoor Air Quality Enhancement
Nestled in the heart of Little Rock, Arkansas, Arkansas Heart Hospital stands as a beacon of excellence in cardiovascular care, having garnered over a decade of accolades for its pioneering advancements in treatment technologies. This nationally recognized and award-winning institution is unwavering in its mission to prevent, diagnose, and treat cardiovascular diseases, proudly holding a place among the top 6 US hospitals for cardiology according to Newsweek and Statista's World's Best Hospitals list.
Beyond its medical prowess, Arkansas Heart Hospital extends its commitment to providing the highest quality care to encompass the optimization of its indoor environment. In 2023, the hospital embarked on a rigorous indoor air quality investigation, guided by the astute expertise of Dr. Martin, an environmental microbiologist of exceptional repute.
With meticulous precision, Dr. Martin delved into the labyrinth of laboratory results, uncovering elevated levels of airborne mold/fungi, general particulate matter, and VOCs (volatile organic compounds) in specific areas of the hospital. Unwavering in his resolve, Dr. Martin meticulously crafted a comprehensive set of protocols to combat these indoor air quality challenges. His recommendations encompassed a multi-pronged approach, including:
* Upgrading the hospital's HVAC system to enhance air filtration capabilities, ensuring the removal of airborne contaminants with enhanced efficiency.
* Implementing stringent cleaning and maintenance procedures to minimize the accumulation of contaminants, fostering a pristine indoor environment.
* Enforcing a rigorous infection control policy to prevent the spread of airborne pathogens, and safeguarding the health of patients, staff, and visitors.
Following the meticulous implementation of Dr. Martin's meticulously devised protocols, Arkansas Heart Hospital underwent rigorous post-intervention testing. The results were nothing short of remarkable, revealing a dramatic reduction, and in some cases, complete elimination of airborne mold/fungi, general particulate matter, and VOCs. The hospital's TVOC (total volatile organic compound) rating soared from "POOR" to "GOOD" and ultimately surpassing even the most stringent EPA/WHO standards.
Dr. Martin's exceptional contributions to improving indoor air quality at Arkansas Heart Hospital exemplify his unwavering dedication to patient safety and well-being. His meticulous approach, coupled with his deep expertise in environmental microbiology, has transformed the hospital's indoor environment, fostering a haven of pristine air quality that promotes healing and recovery. Arkansas Heart Hospital stands as a testament to Dr. Martin's exemplary leadership and the hospital's unwavering commitment to providing a safe and healthy environment for its patients, staff, and visitors.
Please take note to the following: Indoor Air Quality (re)testing took place throughout the interior space of the Arkansas Heart Hospital. The purpose was two-fold: first, we needed to identify the nature and extent of any potential airborne mold/fungi, non-viable particulate matter that can act as allergens (dander, fiber glass, pollen, dust mites, etc.), and chemical compounds.
The second purpose was to compare the findings to the conditions that were present prior to the installation of the M3 System diffuser to determine its effectiveness. The testing was scheduled approx. 8 weeks after original M3 System installation, and most samples were taken in the exact same locations as the pre-installation testing for as much comparative accuracy as possible.
Air sampling identified each airborne mold spore by species and quantified them by concentration level in the unit of measurement “spores per cubic meter” of air (spores/m3). Also identified and quantified in each air sample: Hyphal fragments, pollen, insect parts, dust mites, hairs, algae, cellulose particles, starch particles, dander (skin cells), fiber glass particles, synthetic fibers, carbon-based particles, and general background debris such as dust/dirt.
Samples were analyzed by one of the nation’s premier IAQ and microbiology laboratories, Eurofins PK Laboratory located in Ft. Lauderdale, FL. Test results indicate the following noteworthy points:
1. Air sample results from the pre-test showed a typical variety of airborne mold/fungal species, as well as a typical variety of nonbiological particulate matter. Anything that was detected that would be considered pathogenic (i.e. Cladosporium and Aspergillus sp.) was found in low levels that are indicative of normal conditions with exception to a couple of samples (Corridor, Nurse’s Station 2nd floor, and Respiratory #2), which were “borderline” in terms of acceptable levels.
2. Pre-test: [Taken from pre-installation report]: Results for the non-biological particulate matter showed a healthy variety of items present, including cellulose fibers, synthetic fibers, starch particles, dander (skin cells), and fiber glass particles. Concentration levels were notably excessive with dander in particular. Also, fiber glass
particles were identified in 5 of the 8 areas checked. This includes sensitive zones such as Respiratory and Wound Care. Concentration levels were moderately high, and with particular note to glass particles, it is preferable to find no glass particles in the air, especially in a hospital setting.
3. Post-M3 installation data shows a dramatic reduction, and in some cases total elimination of, airborne mold/fungi, general particulate matter, as well as VOCs (chemical based (Volatile organic compounds’).
Airborne Concentration Levels in Context:
NOTATIONS
i. = Pre M3 System Installation and Activation
ii. = Post M3 System Installation and Activation
1. Mold/Fungi:
(spores/m3 = number of spores per cubic meters of air. Not to be confused with the M3 System machine)Lobby: Main
i. 590 spores/m3 pre-installation
ii. 27 spores/m3 post-installation
Corridor: Level 1 Near Cafeteria
i. 2,000 spores/m3 pre-installation
ii. 0 spores/m3 post-installation
Nurse’s station: Level 1
i. 1,000 spores/m3 pre-installation
ii. 0 spores/m3 post-installation
Respiratory:
i. 53 spores/m3 pre-installation
ii. 13 spores/m3 post-installation • Penicillium/Aspergillus
Lobby: Level 1 Entrance
i. 110 spores/m3 pre-installation
ii. 0 spores/m3 post-installation
Corridor:
i. 110 spores/m3 pre-installation
ii. 0 spores/m3 post-installation
Nurse’s station:
i. 370 spores/m3 pre-installation
ii. 0 spores/m3 post-installation
Respiratory:
i. 210 spores/m3 pre-installation
ii. 0 spores/m3 post-installation
2. Non-viable particulate matter:
• DanderEngineering:
i. 6,000/m3 pre-installation
ii. 130/m3 post-installation
Wound Care:
i. 4,200/m3 pre-installation
ii. 120/m3 post-installation
Pre-Admin:
i. 3,500/m3 pre-installation
ii. 210/m3 post-installation
Corridor L2:
i. 3,400/m3 pre-installation
ii. 80/m3 post-installation
Respiratory:
i. 6,100/m3 pre-installation
ii. 130/m3 post-installation
Nurse’s Station:
i. 3,100/m3 pre-installation
ii. 40/m3 post-installation
Admin:
i. 2,800/m3 pre-installation
ii. 67/m3 post-installation
Fiber glass particles:
Originally identified in 5 of 8 samples, and were completely eliminated in post test samples.• Other miscellaneous airborne particles identified in the pre-installation of the M3 System units such as Starch Particles, Cellulose fibers, Synthetic Fibers, etc. were all virtually eliminated or found in such minor levels that their presence is insignificant.
• The “Background Debris” reading on all air samples taken prior to the M3 System installations showed a 3+ reading out of 4+ [readings go from 1, to 1+, to 2, 2+, 3, 3+, 4, and 4+). This indicates a very high amount of dust & dirt from the air was present in the samples as “background debris” on top of everything else identified. The post-installation testing showed every “background debris” reading to be “<1+” which indicates the overall cleanliness of the air in general, and verifies that the M3 System and micro-vaporized product are removing these particles from the air.
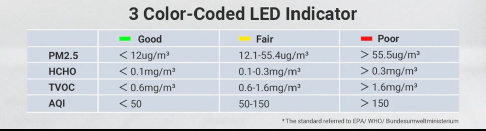
*HCHO: Formaldehyde
*PM2.5: refers to fine inhalable particles w/ diameters that are generally 2.5 micrometers & smaller.
*TVOC: Total VOCs
* Total initial VOC (TVOC) count: 2.54 micrograms
*Acceptable limit for HCHO (Formaldehyde) = below 0.1 micrograms
Post-test #1 @ 10 weeks:
Basement/Engineering:
AQI: 8
HCHO: 0.07
PM2.5: 2
TVOC: 0.37
Admin 3rd Floor:
AQI: 4
HCHO: 0.09
PM2.5: 1
TVOC: 0.52
Post-test #2 @ 15 weeks:
Basement/Engineering:
AQI: 4
HCHO: 0.04
PM2.5: 2
TVOC: 0.18
Admin 3rd Floor:
AQI: 4
HCHO: 0.03
PM2.5: 2
TVOC: 0.18
Contact Us
OFFICES LOCATED IN:
North Miami, Florida
Bluffton, South Carolina
Tel: 843-368-7063